Peyer Patches, Tiny Tonsils In Your Small Intestine Are Part Of The Disease
Tonsils are the principal source of IgA antibodies that attack the kidneys of people with IgA Nephropathy
Tonsils, and it seems Peyer’s Patches in the small intestine, sit patiently and when harmful bacteria pass by they trigger the production of IgA.
They are the first line of defense, but for people with Berger’s Disease the defense is too much for our kidneys
By tending to the garden that is our gut and its flora and fauna we just might help cure the disease.
Tonsils and it seems their closely related Peyer’s Patches, are the first part of our immune system that ‘sees’ incoming bacteria, virus, and irritants that our immune system has evolved to protect us from. The tonsillar tissues, part of Wagner’s Ring that includes adenoids, are at the back of our throat. As almost everything that comes into our bodies must pass by they are able to rapidly react. That reaction to agents of potential harm, antigens, comes in the form of the production of the primary antibody, IgA.
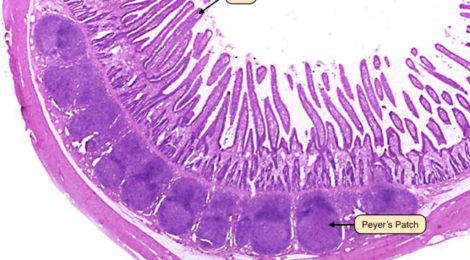
Tonsils not only ‘see’ and react to passing antigens, they are soft spongy tissue with pockets, crypts, where bacterial agents can lodge and grow. This is like having your own med lab in your throat that cultures bacteria and identifies friends from foes. The foes are attacked by the tonsils that pump sticky IgA into our blood. Likewise, Peyer’s Patches are at the beginning of the intestinal tract, just where the chemistry changes from the powerful acid enzyme stomach digesting engine. Any bacteria or pathogen making through the stomach is quickly identified and acted upon by the Peyer’s Patch immune tissues.
For those with IgA Nephropathy we are vulnerable to that dimeric and polymeric IgA, large sticky molecules, that clump and irritate our delicate kidney membranes. These ‘clumps’ are what forms the ‘crescents seen in an IgAN patients biopsy. While removing one’s tonsils is a proven effective treatment to limit sticky IgA for IgA Nephropathy patients that surgical option is not available for the related Peyer’s Patch problem.
The connection between a dysregulated gut-associated lymphoid tissue and IgA nephropathy (IgAN) was postulated decades ago after the observation of the association of IgAN with Celiac disease. Pivotal studies have shown a role for alimentary (aka tonsillar) antigens, in developing IgAN. A reduction in IgA antigliadin antibodies and proteinuria was reported after gluten free-diet in patients with IgAN.
Peyer’s Patches, that are located in the small intestine are essentially a micro-analog of our tonsils and adenoids. They are similar in physical form, albeit much smaller, and importantly are a thymus-derived part of our immune system. The thymus immune system is considered the primitive immune system. Mother Nature rarely gets rid of things that work like the thymus-derived immune system even though she has supplemented and improved upon it with the modern immune system that resides largely in our bone marrow. Our primitive immune system makes big sticky IgA where the modern immune system makes monomeric, small molecule, less sticky IgA.
Recently a genome-wide association study showed that most genetic loci associated with IgAN also are associated with immune-mediated inflammatory bowel diseases, maintenance of the intestinal barrier, and response to gut pathogens. Transgenic mice that overexpress the B-cell activating factor develop hyper-IgA with IgAN modulated by alimentary components and intestinal microbiota. It appears likely that a soluble form of the IgA receptor (sCD89) develops as IgAN. It, in turn, is regulated by dietary gluten.
New drug treatment is the pharmaceutical equivalent to a ‘tonsillectomy’ for Peyer’s Patches.
Recent observations have confirmed gut-associated lymphoid tissue hyper-reactivity in IgAN patients with IgA against alimentary components. This has led to drug development that targets Peyer Patches as a means to suppress the thymus-derived forms of IgA. There are Interesting results provided by the NEFIGAN randomized controlled trial, which adopted an enteric controlled-release formulation of the corticosteroid budesonide targeted to Peyer’s patches. After 9 months of treatment, a reduction in proteinuria was observed with stabilized renal function and limited adverse events. The gut-renal connection is an area of promising new treatment approaches for patients with IgAN.
This emerging science leads one to imagine that IgAN patients might well consider a gluten-free diet and become much more aware of our individual gut biota. Without gluten to host gut biota that stimulates our Peyer Patches into action and by seeding our gut with ‘good biota’ we might well add another potent treatment to sustain our health and kidneys.
I’d be interested in hearing from IgAN patients who have noticed the pros and cons of gluten-free diets and information on their preferred but biome constituents.

Recent Comments